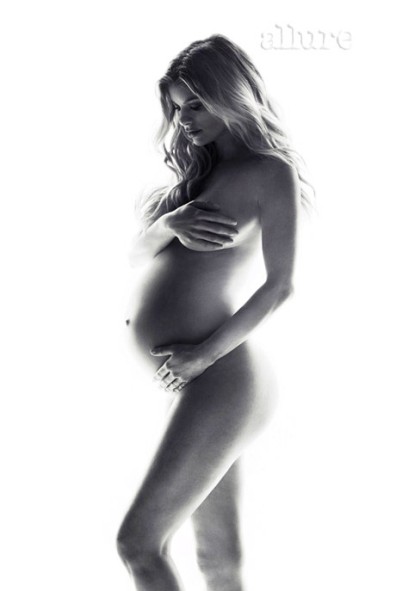
For first-time moms or women who have high-risk pregnancies, the idea of prenatal testing can be scary and overwhelming. Dr. Myra Wick of the Mayo Clinic shares some of the most important questions couples should ask.
The issue of prenatal screening seemed pointless. My husband and I were ecstatic to welcome our child and while we, like every expectant parent, prayed for a healthy baby, we knew if something was “wrong,” it wouldn’t matter. Our baby was our baby.
First-trimester screening
It’s interesting to note that the ultrasound screenings I underwent in the first trimester of my pregnancy showed nothing abnormal.
First-trimester screening, which includes an ultrasound to examine the nuchal translucency and the level of two markers in the mother’s blood, has a detection rate for Down syndrome of approximately 85 percent, with a 5 percent false positive rate.
In addition, according to Dr. Myra Wick of the Mayo Clinic in Rochester, Minnesota, who is board-certified in both OB-GYN and Medical Genetics, “Advanced level ultrasound in the second trimester will detect approximately 50 percent of cases of Down syndrome. Patients most commonly move forward for additional reassurance.”
It wasn’t until we received the results from blood screening that we became concerned.
According to the Mayo Clinic Guide to a Healthy Pregnancy, first trimester screening test results are “considered positive for Down syndrome if the risk is 1 in 230 or greater.”
Blissful ignorance?
I have to admit, I had a nagging sense early on that something was wrong, even before we received the results of the first screening test, which shared the likely chances that our baby would have a genetic disorder.
Hearing those numbers for the first time wasn’t as scary as they might be now, simply because I didn’t know what a high-risk ratio sounded like. Our genetic counselor told us our unborn child had a one in 13 chance of having something called Trisomy 18.
To me, a former journalist who avoids math like cats avoid water, well, heck, that wasn’t so bad, right? I mean, if the baby’s chances were one in 13, that meant there were 12 other shots that things would be just fine. Right?
I was uneducated on the risks of genetic conditions, and I realize now that ignorance wasn’t bliss but rather a much more moderated panic.
Our baby’s risk of having Down syndrome was in the single digits . Basic research told us that Trisomy 18 came with a high risk of intrauterine death, or death the within the first year of life. People with Trisomy 21 had a life expectancy of 60 years.
I prayed for Down syndrome.
{pageBreak}
Weighing risk vs. 'yes or no' answers
Ultrasound FAQs
Dr. Wick recommends asking these questions after a patient undergoes an ultrasound:
- Are there anomalies on the ultrasound?
- If anomalies exist, will the fetus be able to survive them in the long term?
- If the fetus is diagnosed with a non-life-threatening disorder but anomalies exist , ask to meet with the neonatologist and appropriate specialists .
The Mayo Clinic also offers an overview of common prenatal tests.
“Risk assessment is a difficult concept for many patients,” Dr. Wick says. “We all have a different perception of what is considered ‘high risk,’ and we all want a definitive yes-or-no answer, not a risk!
“Some patients consider 1/200 to be unacceptably high, and will proceed with testing. I have also had patients with a much higher risk, 1/25, decide that this is not high enough to proceed with additional testing,” Dr. Wick continues.
“The decision to proceed or not may be based on how the patient/couple will manage the pregnancy,” Dr. Wick says. “If termination is a consideration, these couples will usually proceed with invasive testing so that further management decisions can be made.
“If couples are not considering termination, then it may be reasonable to weigh the risks of the procedure versus the risk that the pregnancy is affected.”
Plan of delivery
Every delivery is different, and each couple must approach delivery with a plan that works for them.
“If the fetus has a lethal condition, it may also be useful to meet with the neonatologist to discuss management at delivery,” Dr. Wick advises. Depending on the baby’s condition, a couple may choose “comfort care” versus multiple interventions.
"You should also discuss plan of delivery with your provider,” Dr. Wick says. “These are obviously very sensitive issues.”
Hearing the results
At the beginning of our pregnancy, my husband and I agreed it didn’t matter what might be different about our child, we looked forward to meeting him or her and starting our family.
When the first screening results came back, the numbers were like an unexpected flare shooting into the sky. We talked at great length about the pros and cons of going further and having diagnostic testing. It was riskier to the baby because diagnostic tests are invasive, whereas the screening I’d undergone to that point was from simple blood tests.
Together, we agreed we wanted to know what was reasonable to find out. We wanted to be prepared, and, as we learned more about Trisomy 18 and Trisomy 21, we realized either scenario came with increased risks of heart defects. We decided we had to know more.
Diagnostic testing
At 18 weeks, I underwent an amniocentesis, a diagnostic test that’s often used to follow up on an abnormal screening test. Diagnostic tests can better confirm genetic conditions.
Dr. Wick explains, “Diagnostic testing is also referred to as invasive testing. This includes chorionic villus sampling and amniocentesis .
“CVS is typically performed between 11 and 14 weeks. It involves taking a small sample of the placenta . This may be done with a needle through the abdomen or by passing a small catheter through the cervix . CVS is done under ultrasound guidance. The quoted risk of pregnancy loss is approximately 1 percent.
“Amniocentesis typically is done at or after 15 weeks and is also usually done under ultrasound guidance," Dr. Wick continues. "Risk of loss is generally quoted as 0.5 percent. Both CVS and amnio obtain fetal tissue, which can be used for chromosome analysis or other genetic testing.”
For us, prenatal testing also helped discover and track our son’s evolving hydrops condition. Hydrops is two or more of the following 1) ascites [fluid collection in the abdomen], 2) pleural effusion [fluid around the lungs] 3) pericardial effusion [fluid around the heart], 4) skin edema [e.g., fluid collection in the extremities, similar to what many women experience late pregnancy but usually more pronounced], 5) polyhydramnios [abnormally increased amniotic fluid].
“Hydrops can be associated with several conditions, including Down syndrome,” Dr. Wick explains, “but it generally carries a poor prognosis.”
{pageBreak}
Discovering a potentially lethal condition
“Prenatal testing can be a very important and emotional decision for parents,” Dr. Wick says. “If the infant has a lethal condition, discussion should include monitoring during labor .
Dr. Wick advises couples to plan ahead for either scenario, whether the child is delivered in good health or something goes wrong and the child does not survive delivery.
Acknowledging how difficult it will be to face these questions, Dr. Wick encourages couples to plan ahead and ask:
- Will there be surgical interventions for a lethal condition or comfort care? “If you are at a small community hospital, your care provider may be more comfortable sending you to a tertiary center where there is more likely to be a ‘bereavement team’ and providers who have special training in the care of these families,” Dr. Wick says.
- If the infant has problems and there will be interventions will there be specialists at the delivery ?
- Antenatal testing , typically with ultrasound and/or monitoring of the infant’s heart rate tracing, can be used to assess for developments such as hydrops or abnormal blood flow in the infant. If the testing is abnormal, and the infant does not have a lethal condition then testing may help the care team make decisions about early delivery.
Learning to breathe smoothly
In our case, our son looked perfectly healthy via ultrasound on a Friday, and by Monday morning had quite a bit of fluid building in his left lung cavity. Our physicians consulted with other physicians in the Northeast and decided we should continue to monitor the situation.
By the following Friday, the fluid had increased, and I was on my way to the hospital. Before Charlie was born at 33 weeks, weighing 4 pounds, 14 ounces, maternal and fetal physicians removed most of the fluid in his lung cavity, in utero.
“The rollercoaster had many curves and many dips„
As I lay staring at one spot on the ceiling and trying to breathe smoothly and evenly, a physician inserted a needle into my abdomen, then into my uterus and into Charlie’s left lung cavity to withdraw fluid.
Twice, my husband watched as a nurse who had become a trusted friend helped guide each physician’s painstaking precision using ultrasound technology.
Those moments were perhaps the most vulnerable I will ever feel as a parent — or I certainly hope so. I was putting my child’s life in doctors’ hands, trusting their skill and expertise.
Trusting your medical team
When Charlie was born, he had a chest tube for one week before the fluid subsided and his lungs remained clear. I’ll never forget the incredible work, patience and compassion of the physicians who monitored Charlie, modified his treatment and ensured he could come home with us one month after he was born.
The rollercoaster had many curves and many dips, but throughout our journey, we had complete confidence in our physician, Dr. David C. Shaver, at Presbyterian Maternal and Fetal Medicine in Charlotte, North Carolina.
He never frightened us, and he never sugarcoated the truth. He asked for our thoughts, and respectfully and delicately shared his professional opinion when we hesitated.
The best illustration of his dedicated demeanor came one afternoon, midway through the pregnancy, when Charlie’s hydrops had resolved almost entirely, which we greeted with wary, nervous joy.
Dr. Shaver sat for what seemed like days, sliding the ultrasound device over my belly, pushing and prodding, then stopping and staring at the computer screens without expression. My husband and I exchanged nervous glances several times, as the exam went on and on.
Becky, our by-now beloved nurse, returned to the exam room and, upon seeing Dr. Shaver still studying the screen, said, “Oh, I didn’t know you were still looking! Everything OK?”
Dr. Shaver nodded. He never looked up from the screen. “Everything looks great,” he said calmly. “I’m just… being paranoid, I guess.”
My husband and I looked at each other, relief escaping audibly from our lips. “Dr. Shaver, you can watch for a week if you want,” I said.
His was the last hand I shook nearly 18 months later, as I prepared to have a scheduled C-section with our second child, our daughter. Parenthood is scary, and the moments leading up to childbirth are a whirlwind. Trusting your physician implicitly makes all the difference.
{pageBreak}
Back to basics
Before undergoing any testing, Dr. Wick says one of the most important questions for a couple to address head-on is how they will use test results. “Will the results change management of the pregnancy ? Does the couple agree on how they will follow up an abnormal test result?”
As Dr. Wick points out, “Some couples have never discussed their thoughts on termination — not all partners agree on this!”
Everyone reacts differently
While my husband and I agreed early on that termination was not an option, we each had very different reactions to prenatal testing and the results we received.
“We are in love with our little boy„
After watching me undergo the amnio procedure, my husband returned to work and promptly Googled support groups for parents of children with Down syndrome. We hadn’t gotten a diagnosis yet, but he was already reaching out.
As fate would have it, a local DADS Group was meeting that very night in a neighboring town, and Jeremy attended. There, he met families who will be part of our lives forever. He found hope and positivity, which was exactly what he needed.
Alternately, I spent months unable to really speak with anyone about the diagnosis for a variety of reasons, mostly because of overwhelming guilt. Fate again intervened when my husband scheduled dinner with two couples from the DADS Group on what turned out to be the night before we learned Charlie’s hydrops had returned.
The next afternoon, I was admitted to the hospital, and three days later, we welcomed our beautiful son.
Only one regret — wasted time
Ours is an ongoing story and, without question, one of the best love stories I’ve ever known. We are in love with our little boy, and everyone who gets to know him has come to understand what an overwhelmingly positive difference he has made in our lives.
I have no regrets about having the prenatal testing done; for better or worse, my husband and I came to terms with the diagnosis at our own pace. Any remaining worry slipped away once we looked at our son and touched his silky skin.
What I do regret is the tremendous amount of time I wasted worrying about what I realize now were baseless concerns. Knowing and loving Charlie outweighs any challenge we may face together.
Read more about prenatal testing
What expecting moms should know about prenatal testing
Are you of advanced maternal age?
What to expect from the 20-week ultrasound