
Parents of children with Down syndrome often think restless sleep patterns are just part of childhood, but research shows real health concerns and causes that can be treated.
Medical reasons
for fitful sleep
Most parents know the mixed feeling of relief and dread as the first light of morning creeps between the blinds after a sleepless night.
Having a child with special needs can be particularly challenging, and sleep issues that are prevalent in children with Down syndrome can be elusive.
Here’s the good news
Knowing what to look for is key. Maybe you’ve already noticed your child sleeping in strange, folded-over positions. Did you chuckle? Post it to Facebook? Marvel at the phenomenon that is low muscle tone?
I did. And then I heard a sleep specialist speak to my local Down syndrome association. Her presentation showed a picture of a child folded over in sleep.
“This is a sign of sleep apnea,” pointed out Dr. Carolyn E. Hart of Presbyterian Sleep Health - Charlotte . While between 2 and 4 percent of “typically developing” children have Obstructive Sleep Apnea , between 30 and 55 percent of children with Down syndrome have OSA.
Why the high incidence?
Individuals with Down syndrome generally have a handful of physical characteristics that increase the risk of OSA, Dr. Hart says. Overwhelmingly, the low muscle tone that often accompanies Ds affects airways. Couple low tone with a larger tongue, a smaller throat and tonsils, and it may seem remarkable the percentage isn’t higher.
What is sleep apnea?
Apnea means disrupted breath. Researchers Amanda Wood and Ben Sacks report children with sleep apnea “may be heard to snore, cough, choke and exhibit signs of restlessness, unusual sleeping positions, excessive sweating and periods when breathing is observed to stop.“
In 2004, Wood and Sacks investigated behavior-related sleep issues, which can be helpful information if a child’s disrupted sleep turns out to be behavioral instead of a health issue.
“A typical apneic episode is when a child stops breathing altogether for a short period of time and then suddenly resumes breathing with rapid gulping for air,“ the study explains.
For more information, visit the National Down Syndrome Association.
Dr. Hart explains that because children with Down syndrome have a less responsive autonomic nervous system, their heart rates don’t adjust before and after apnea occurs, and their oxygen levels dip deeper and longer than when apnea occurs in children who do not have Down syndrome.
Don’t mistake deprivation for disability
If a child’s breathing is interrupted during sleep, then a child’s sleep is interrupted. Sleep deprivation can have some obvious symptoms, but they may not seem so distinct in children with intellectual disabilities such as those that can occur with Down syndrome.

“So many things are mistaken for intellectual disability with our kids when some of it can be medical and can be treated,” shares Melanie, whose daughter was diagnosed with apnea after a sleep study at 3-1/2 years old.
“I just thought she was a mellow kid who liked to sleep. Poor thing was sleep deprived. Her oxygen levels were what they were [before she had] heart surgery! Imagine how that affects cognition?”
Melanie never suspected her daughter’s apnea and didn’t think a sleep study was necessary.
“I'm well-educated, involved, curious, etcetera,” she says, “and I sincerely did not believe she had [apnea].”
A sleep study showed Melanie’s daughter’s breathing was obstructed five times every hour for up to 20 seconds at a time.
Their ear, nose and throat specialist recommended a tonsillectomy and adenoidectomy, which were performed about a year ago. Today, “the difference in her energy level [is] incredible!” Melanie shares.
Dr. Hart recommends undergoing a sleep study before any surgeries to ensure all possible issues are identified first.
Not every sleep study results in a diagnosis that requires drastic measures. Julie’s daughter was 3 years old when she underwent a sleep study. “She snores and sleeps in odd positions to get best amount of air and wakes once or twice in the night, so we wanted to check to be sure. But she is always fully rested upon waking, which is important.“
The sleep study showed Julie’s daughter did not have low oxygen levels and she didn't wake too often, so no follow-up was needed.
Periodic Limb Movement Disorder
“[My daughter] has always been what I term a ‘wild sleeper,’” Terri says. “We would hear her thrashing around in the bed and even falling out of bed a few times.”
Terri and her daughter, who has Down syndrome, have endured two sleep studies; the first study didn’t produce enough data. “All the wires and monitors really freaked her out and she's usually pretty mellow,” Terri explains. Her daughter wasn’t able to sleep enough to produce substantive data the first time.
Luckily, their second sleep study went more smoothly. “She was still not happy about the wires, but we gave her melatonin this time to get her to fall asleep,” Terri says.
This time, the study showed Terri’s daughter does not have apnea but likely has Periodic Limb Movement Disorder, which is characterized by more than four movement-related awakenings during an hour of sleep.
While iron supplements sometimes can help, they can take several months to take effect. “We're just waiting now to see if this works,” she says.
What is a sleep study?
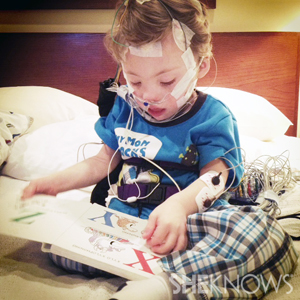
For a child with Down syndrome, a sleep study is an overnight opportunity for physicians to capture helpful data to determine if a sleep disorder exists, and if so, to what extent. A parent accompanies the child to a clinic, where technicians will attach electrodes to the child’s head and even under the child’s nose, to capture breathing data.
Parents share sleep study tips
Before you go:
- Doctors and parents agree: Younger children handle sleep studies easier. The recommended age is 3 years old.
- Keep perspective! “It's certainly important enough to go through the hassle,” Julie points out. “It's just one night!”
What to bring:
- Relaxing music
- A familiar blanket or pillow
- Children's books to read while electrodes are applied
Once you’re there:
- Ease the child into the process, recommends Tamara, whose son has Down syndrome and has undergone a sleep study. “The tech started putting ’stickers’ on him without any interaction. If I had to do it again… I would ask where things need to go, and then do it myself. You know your child and he trusts you.
- Ask if the lead ’stickers’ can be attached before the wires. “One hurdle at a time!“ Tamara advises.
Once it’s over:
- “Don’t plan on a post-study breakfast date!” Tamara warns. Your child’s hair will be covered in the goop required to keep the leads attached and working.
- Plan on two baths, using hot water to remove the “goop.”
- Your child's head will be wet, so plan accordingly and bring extra clothes and a hat if wintertime.
More about Down syndrome
Nonprofit film turns camera on teens with Down syndrome
Moms share favorite books on Down syndrome
Imagining a future for my son with Down syndrome